Mallet toe is another name for the foot condition that is known as hammertoe. It is an ailment that prevents the toes from straightening out, and they can bend at a downward angle. The toes that are generally affected are the second, third, or fourth toes, and in severe cases, surgery may be necessary to restore the toes back to a normal position. The reasons many patients develop hammertoe can include wearing shoes that do not fit correctly, an abnormality in the toe muscles and tendons, or medical conditions such as arthritis. Calluses or corns may form on top of the affected toes, and this can be a result of excess friction that is caused by wearing tight shoes. If you notice the first stages of hammertoe developing, it is strongly suggested that you speak to a podiatrist, who can determine what the best course of treatment is for you.
Mallet toe is another name for the foot condition that is known as hammertoe. It is an ailment that prevents the toes from straightening out, and they can bend at a downward angle. The toes that are generally affected are the second, third, or fourth toes, and in severe cases, surgery may be necessary to restore the toes back to a normal position. The reasons many patients develop hammertoe can include wearing shoes that do not fit correctly, an abnormality in the toe muscles and tendons, or medical conditions such as arthritis. Calluses or corns may form on top of the affected toes, and this can be a result of excess friction that is caused by wearing tight shoes. If you notice the first stages of hammertoe developing, it is strongly suggested that you speak to a podiatrist, who can determine what the best course of treatment is for you.
Hammertoes can be a painful condition to live with. For more information, contact Jeffrey Parrett, DPM of Parrett Podiatry. Our doctor will answer any of your foot- and ankle-related questions.
Hammertoe
Hammertoe is a foot deformity that occurs due to an imbalance in the muscles, tendons, or ligaments that normally hold the toe straight. It can be caused by the type of shoes you wear, your foot structure, trauma, and certain disease processes.
Symptoms
- Painful and/or difficult toe movement
- Swelling
- Joint stiffness
- Calluses/Corns
- Physical deformity
Risk Factors
- Age – The risk of hammertoe increases with age
- Sex – Women are more likely to have hammertoe compared to men
- Toe Length – You are more likely to develop hammertoe if your second toe is longer than your big toe
- Certain Diseases – Arthritis and diabetes may make you more likely to develop hammertoe
Treatment
If you have hammertoe, you should change into a more comfortable shoe that provides enough room for your toes. Exercises such as picking up marbles may strengthen and stretch your toe muscles. Nevertheless, it is important to seek assistance from a podiatrist in order to determine the severity of your hammertoe and see which treatment option will work best for you.
If you have any questions, please feel free to contact our office located in Waxahachie, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Hammertoe is a foot deformity that occurs due to an imbalance in the tendons, muscles, or ligaments that are responsible for holding the toes in their normal position. This condition may be caused by poor footwear, foot structure, trauma, and disease. The most common solution for hammertoe is to relieve the pain by changing your footwear and wearing orthotics. In severe cases, surgery may be required.
The shoes that are most likely to cause hammertoe are high heeled shoes or shoes that are too tight in the toe box. Tight shoes will force your toes to crowd together in a curled position. This position will likely continue when you take your shoes off. Another cause is trauma. When you stub your toe, you are increasing the chance that you will develop hammertoe.
There are risk factors that may make you more likely to develop this condition. Women are more likely to have the condition compared to men, and it is also more likely to appear in those who are older in age.
Many different foot problems can be avoided by wearing shoes that have adjustability, adequate toe room, and low heels. Furthermore, if you want to buy new shoes, you should look to purchase them at the end of the day and make sure you know your correct size. The importance of buying shoes at the end of the day is that your feet swell as the day progresses. You should also ensure that you are wearing your correct size because your shoe size may change as you grow older.
To diagnose someone with hammertoe, your podiatrist will need to conduct a thorough examination of your foot. Your doctor may even order an x-ray to evaluate the bones and joints of your feet and toes.
If you have hammertoe, your podiatrist may recommend that you wear shoes that fit you better along with inserts to place inside them. Additionally, he or she may suggest special exercises for you to perform to stretch your toes. One helpful exercise it to pick up marbles with your feet or crumple a towel with your toes.
Prior to meeting with your podiatrist, it will be helpful to make a list of all the symptoms you are experiencing. You should also make a note of medications you are taking and important personal information about your medical history.
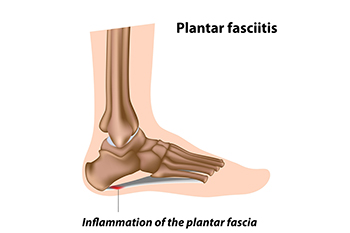
Plantar fasciitis is caused by inflammation of the plantar fascia, a thick band of tissue connecting the heel to the toes. Risk factors include obesity, prolonged standing, high impact activities, flat feet, high arches, and tight calf muscles. Symptoms often involve sharp heel pain, especially with the first steps in the morning or after periods of rest, as well as swelling and stiffness. Causes include overuse, poor footwear, sudden increases in activity, or biomechanical imbalances. A podiatrist can diagnose the condition, recommend supportive footwear or orthotics, provide stretching exercises, and offer treatments to reduce inflammation and restore mobility. If you have heel pain, it is strongly suggested that you promptly contact a podiatrist who can accurately diagnose and treat what may be going on.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Jeffrey Parrett, DPM from Parrett Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions, please feel free to contact our office located in Waxahachie, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
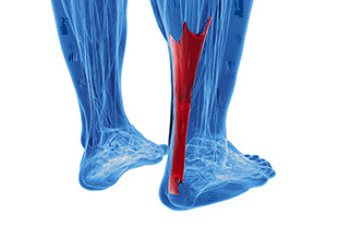
Achilles tendonitis occurs when the thick tendon that connects the calf muscles to the heel bone becomes inflamed from overuse or strain. This tendon plays a key role in walking, running, and pushing off the toes, which makes it vulnerable to injury from repetitive motion or sudden increases in activity. Common causes of Achilles tendonitis include running on hard surfaces, training without proper warm-up, and wearing shoes that lack adequate support. Flat feet, bone spurs on the heel, and certain health conditions can increase the risk of Achilles tendon irritation. Symptoms include pain or stiffness in the back of the ankle, swelling, warmth, and difficulty standing on the toes. Morning stiffness is especially common. If left untreated, inflammation may progress to tendinosis, where the tendon begins to degenerate. In severe cases, a rupture may occur and require surgery. If you are experiencing symptoms of Achilles tendonitis, it is suggested that you make an appointment with a podiatrist for an exam and treatment.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact Jeffrey Parrett, DPM of Parrett Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact our office located in Waxahachie, TX . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Tendons are fibrous tissues that connect muscles with bone. The Achilles tendon is the largest tendon in the body. It connects the calf muscles at the back of the leg with the heel, and facilitates movements such as jumping, running, and walking.
Because the Achilles tendon is engaged so frequently and bears a great deal of pressure and stress throughout the day, it can become injured. Achilles tendon injuries cause the tissue to become irritated, inflamed, and swollen. Pain can come on gradually or be immediate, and will vary from mild to severe depending upon the injury. Where the pain occurs will vary as well, from just above the heel up through the back of the leg. There may also be stiffness in the tendon.
Achilles tendon injuries can often be caused by repetitive stress. They may also occur while running, playing tennis, gymnastics, football, basketball, dancing, soccer, baseball or other sports that require speeding up, slowing down, or pivoting quickly. Wearing high heels, falling from an elevation, stepping in a hole, having flat feet, bone spurs, tight leg muscles or tendons, wearing improper athletic shoes, exercising on uneven surfaces, or starting a new type of exercise can also cause Achilles tendon injuries.
The two most common Achilles tendon injuries are tendonitis and ruptures. Tendonitis causes painful inflammation and can occur in different parts of the tendon. Non-insertional Achilles tendonitis occurs when the fibers in middle of the tendon begin to break down, thicken, and swell. This condition typically affects younger, more active adults. Insertional Achilles tendonitis occurs where the tendon inserts into the heel bone. It is common for bone spurs to form with this type of injury. This condition can affect people of any age and level of activity.
Achilles tendon ruptures are a tear in the tendon. These breaks may be partial or complete. There may be an audible popping noise at the moment of injury and the pain will be sudden and severe.
An Achilles tendon injury can be diagnosed by your podiatrist after they examine you, check your range of motion, and possibly perform a calf squeeze test or review an X-ray or MRI. Depending on the type and severity of your injury, your podiatrist may treat your condition with rest/ice/compression/elevation (RICE), nonsteroidal anti-inflammatory medications, heel lifts, and stretching and strengthening exercises. If you have torn your Achilles tendon, treatment may include physical therapy, ultrasound, shockwave therapy, or possibly even surgery.

Stress fractures in the feet are hairline cracks in the bone that often develop from repetitive force, rather than a single traumatic event. Stress fractures generally occur in the long bones of the foot, which endure significant impact during walking, running, and jumping. Overtraining, sudden increases in activity, or inadequate rest between workouts raise the risk. Foot structure also plays a role, with flat feet, high arches, or rigid arches contributing to uneven distribution of pressure that can stress certain bones. People with osteoporosis or low bone density are at higher risk, and nutritional deficiencies, such as inadequate calcium or vitamin D, may weaken bone strength. A podiatrist can confirm a diagnosis through examination and imaging, recommend appropriate footwear or orthotics, and advise whether surgery is required in severe cases. If you have symptoms of stress fractures in your feet, it is suggested that you make an appointment with a podiatrist for an exam, diagnosis, and treatment.
Stress fractures occur when there is a tiny crack within a bone. To learn more, contact Jeffrey Parrett, DPM from Parrett Podiatry. Our doctor can provide the care you need to keep you pain free and on your feet.
How Are They Caused?
Stress fractures are the result of repetitive force being placed on the bone. Since the lower leg and feet often carry most of the body’s weight, stress fractures are likely to occur in these areas. If you rush into a new exercise, you are more likely to develop a stress fracture since you are starting too much, too soon. Pain resulting from stress fractures may go unnoticed at first, however it may start to worsen over time.
Risk Factors
- Gender – They are more commonly found in women compared to men.
- Foot Problems – People with unusual arches in their feet are more likely to develop stress fractures.
- Certain Sports – Dancers, gymnasts, tennis players, runners, and basketball players are more likely to develop stress fractures.
- Lack of Nutrients – A lack of vitamin D and calcium may weaken the bones and make you more prone to stress fractures
- Weak Bones – Osteoporosis can weaken the bones therefore resulting in stress fractures
Stress fractures do not always heal properly, so it is important that you seek help from a podiatrist if you suspect you may have one. Ignoring your stress fracture may cause it to worsen, and you may develop chronic pain as well as additional fractures.
If you have any questions please contact our office located in Waxahachie, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Our bones are important aspects of our body and they are constantly changing. The heavier the workload for a bone, the more likely it is that calcium will be placed in it. When a bone isn’t used often, there won’t be much calcium within it. When stress from repetitive loads prevent the bone from being able to repair itself, cracks will start to form. Stress fractures are defined as cracks in a bone that result from repetitive force, such as overuse.
The most common cause of stress fractures is a sudden increase in intensity and duration of physical activity. For example, if you begin to run long distances without working your way into doing so, you will be more likely to develop a stress fracture.
Common symptoms of stress fractures are pain and swelling near the weight bearing area on the injured bone. When initial x-rays are performed, it is possible that the fracture will not show up. However, once the stress on the area continues, the damage will increase, and the fracture will be severe enough to show up on an x-ray. Certain parts of the foot are more likely to develop stress fractures than others. Areas that typically have these fractures are: the metatarsals, the navicular bone, the calcaneus, tibia, and fibula.
Since women are at an increased risk of developing osteoporosis, they are twice as likely as men to sustain a stress fracture. Additionally, old age causes a decrease in bone mineral density which is why elderly people are also likely to develop these fractures.
It is important for you to be professionally diagnosed by a podiatrist if you suspect you have a stress fracture, because there are other injuries that can easily be mistaken for a fracture. Sprains, strains, shin splints, plantar fasciitis, and Morton’s neuroma can all easily be mistaken for stress fractures in the foot. Your podiatrist will likely ask you a series of questions to determine what type of pain you are experiencing. These questions will help your doctor identify whether you have a stress fracture.
The best method of treatment for a stress fracture is rest. Additionally, a walking boot, cast, or crutches, will help rest the area that is injured. The typical healing time for stress fractures is 4-12 weeks, however this depends on which bone is involved.

Excess body weight places added stress on the feet, which can lead to discomfort and reduced mobility. Research shows that carrying higher fat mass is strongly linked to foot pain, while overall body weight can negatively affect how the foot functions during walking and standing. With obesity rates rising across the globe, problems such as plantar heel pain, tendon strain, and joint stress in the feet are becoming more common. This makes awareness and early intervention especially important. Podiatrists play a key role not only in treating foot pain but also in addressing its contributing factors. By working with patients and collaborating with other health professionals, podiatrists can help manage both the mechanical strain on the feet and the broader health issues connected to weight. If you are experiencing foot pain related to weight, it is suggested that you consult a podiatrist for evaluation and care.
Obesity has become very problematic at this point in time and can have extremely negative effects on the feet. If you’re an obese individual and are concerned about your feet, contact Jeffrey Parrett, DPM from Parrett Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Obesity and Your Feet
Since your feet are what support your entire weight when standing, any additional weight can result in pain and swelling. Being overweight is one of the main contributors to foot complications.
Problems & Complications
Extra Weight – Even putting on just a few extra pounds could create serious complications for your feet. As your weight increases, your balance and body will shift, creating new stresses on your feet. This uneven weight distribution can cause pain, even while doing the simplest tasks, such as walking.
Diabetes – People who are overweight are at serious risk of developing type-2 diabetes, which has a drastic impact on the health of your feet. As you get older, your diabetes might worsen, which could lead to loss of feeling in your feet, sores, and bruises. You could also become more prone to various infections.
Plantar fasciitis – Pressure and stress that is placed on muscles, joints, and tendons can trigger plantar fasciitis, which is an inflammation of tissue that forms along the bottom of the foot.
If you have any questions, please feel free to contact our office located in Waxahachie, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.